Category Archives: Uncategorized
The Manchester Cleaning Show 2020

As a board member of the British Cleaning Council the BTA is delighted to support the Manchester Cleaning Show event and has provided you with a LINK to the show webpages. Hope this is helpful !
Manchester Cleaning Show is going virtual
from 14-15 October 2020
We don’t want to wait until September 2021 to see you all again. Our exhibitors have products that can help the UK get back to business now; and so many individuals need the support and the contacts that this event brings. The UK cleaning industry has demonstrated resilience, adaptability, and innovation throughout this pandemic, and there is a wealth of recent experience to share. So we are staging a virtual version of the Manchester Cleaning Show from 14-15 October 2020.
The opportunities that this virtual event presents are exciting and we have a really innovative platform to show you. There are no apps to download and you can view everything on a device of your choice.
So register to join us for free today.
And we look forward to seeing you online in October.
Michelle Andrews
Sales Manager
Non-Domestic Rating (Public Lavatories) Bill

Non-Domestic Rating (Public Lavatories) Bill – Third reading in Parliament on 03 September 2020. Proposed by The Minister of State, Ministry of Housing, Communities and Local Government (Mr Simon Clarke)
Considered in Committee
[Dame Rosie Winterton in the Chair]
12.41 pm
The First Deputy Chairman of Ways and Means (Dame Rosie Winterton)
I should explain that, in these exceptional circumstances, although the Chair of the Committee would normally sit in the Clerk at the Table’s chair during Committee stage, in order to comply with social distancing requirements, I will remain in the Speaker’s chair, although I will be carrying out the role not of Deputy Speaker but of Chairman of the Committee. We should be addressed as Chairs of the Committee, rather than as Deputy Speakers.
Clause 1
Relief from non-domestic rates for public lavatories
Kate Hollern (Blackburn) (Lab)
I beg to move amendment 1, line 6, after “day,” insert
“the hereditament is a publicly-owned library or community centre or a local authority property that is free of charge to enter and contains a public lavatory that is free of charge for anyone to use, or”.
This amendment would extend the rate relief to publicly-owned libraries and community centres, and local authority properties, which are free to enter and which contain public lavatories that are free to use.
The First Deputy Chairman
With this it will be convenient to discuss the following:
Amendment 2, page 1, line 7, after “lavatories”, insert
“which are free of charge for anyone to use”.
This amendment would confine the rate relief to public lavatories that are free of charge to use.
Amendment 3, page 1, line 8, after “zero”, insert
“; and where, on a chargeable day, the hereditament consists partly of public lavatories, the chargeable amount for the chargeable day of the public lavatories shall be separately calculated and the chargeable amount for the chargeable day of the hereditament shall be reduced by the amount calculated in respect of those public lavatories.”This amendment would give rate relief to premises that consist partly of public lavatories according to the proportion of the premises occupied by those lavatories.
Clause stand part.
Clauses 2 to 4 stand part.
New clause 1—Assessment of the impact of Act on provision of public lavatories—
“The Secretary of State must within one year of Royal Assent conduct and publish an assessment of the impact of this Act on the provision of public lavatories.”
This new clause would require the Government to publish a report on the impact of the Act on provision of public lavatories.
Kate Hollern
I pay tribute to my hon. Friend the Member for Bristol West (Thangam Debbonaire) for seeing the Bill through Second Reading with such enthusiasm, and I thank the Clerk of Bills, whose support has been, and continues to be, invaluable.
Public loos have been an integral part of our local communities for more than 150 years, in green spaces and on high streets and thoroughfares. In 1851, London’s Hyde Park welcomed more than three quarters of a million people to the Great Exhibition. The park gave organisers the space to absorb the vast numbers, but visitors presented a public health challenge, and so, in Victorian England, public conveniences as we know them were born. Several years later, in 1858, the man charged with supplying the loos at the Great Exhibition, George Jennings, wrote to the commissioner of sewers offering to set up public conveniences across the City of London.
Back then, conveniences were the preserve of men, but thankfully we have come a long way since then. However, anyone who has ever needed a toilet in public will know that public conveniences are no longer convenient, since there are simply not enough of them. The role of public loos in improving hygiene and health is more important now than ever, given the importance of maintaining high hygiene standards and access to appropriate toilet and hand-washing facilities in keeping covid-19 at bay.
Everyone needs to use the loo, which is a human right under the United Nations sustainable development goals. Women and girls in particular need somewhere to change their sanitary products; people with certain disabilities require accessible toilets, or more frequent use; while parents need to change young children. People who work outside, and homeless people who are now being turfed out of emergency accommodation and back on to the streets, also need somewhere to use the loo. Not only is the lack of loos a public health crisis waiting to happen, but the lack of loos on our high streets, in green spaces and elsewhere is a deterrent to participating in public life for those of us who want to visit our cities, towns and attractions. Some call this a “urinary leash”, with people not feeling comfortable leaving their homes at the thought of being caught wanting in public and with no access to a loo.
Of course, closing public loos has not stopped people needing them; it has just created additional barriers to access for those who need them most. According to the Royal Society for Public Health, the treatment of natural bodily functions as something altogether taboo has proved the touchpaper for ignoring public loos for what they really are—a vital public health resource. The lack of attention paid to public toilets, if you will indulge me, Dame Rosie, is quite frankly potty.
As a constructive Opposition, we on these Benches broadly support the Bill, as we have consistently made clear, since it helps address some of the problems in financing the upkeep of public lavatories. We will not stand in its way or push the amendments to a vote.
However, in many respects the Bill is no more about loos than it is about local government funding—or the lack of it: the fact that it has been brought before the House is a reflection of the need to prop up council finances. After a decade of austerity, councils simply do not have the cash to run public loos, which are estimated to cost between £15,000 and £60,000 each year just to maintain.
Since 2010, public loos have closed at an alarming rate, with over 700 council-run loos closing in the following eight years. Although I appreciate that the Bill came before the House prior to the pandemic, it is curious that the Government have not extended its reach at a time when they are encouraging everyone to get out more. There is nothing in the Bill that would help struggling councils restore or provide additional cleaning and staffing during this crisis, nor does the Bill redress the longer-term damage that the lack of public toilet provision has done over the past decade.
I now move beyond the narrow focus of the Bill; I have already placed my concerns on the record. Although the Bill is important, it is curious that this matter has been prioritised rather than other urgent needs. The renter’s rights Bill promised in the Queen’s Speech is just one example of legislation that the Government could and should have brought forward. Now that we are here, however, I share the ambition of Members on the Conservative Benches to widen access to public lavatories, and I appreciate that the Bill intends to do that. Given that it is before us, we have tabled three amendments and a new clause, which have been grouped. I hope they are taken in the constructive manner intended.
First, I would like to see the Bill extended to provide relief to publicly owned libraries and community centres as well as local authority town halls, which are free for anyone to enter and contain public lavatories that are free for anyone to use. Widening access should be our overriding priority. As the hon. Member for Thornbury and Yate (Luke Hall), the Minister for rough sleeping and housing, made clear on Second Reading, we must support facilities that exist where there are unlikely to be other publicly available toilets or where removing additional costs of business rates could make a real difference to their ability to stay open. That is why I have introduced one of my amendments.
Community centres, libraries and town halls are often conveniently located at the heart of our communities. In my constituency of Blackburn, there are eight community centres, four libraries and three town halls, which cost the council about £400,000 over the course of a financial year. If each of those premises provided a public lavatory, up to an additional 15 loos would be available to the public. The point is that we do not have to build new loos to widen access; we just have to make existing loos more accessible.
Secondly, in return for providing a free-to-use public convenience, each library, community centre and town hall should be eligible for relief equivalent to the rateable value of their public toilets. That would ease the crippling burden on councils, and that money could be better spent on services our communities desperately need. The money saved could pay towards an additional refuse collector or social worker; it could support a food bank or a family fleeing domestic violence.
Thirdly, we want to do away with a fee to pee. Stand- alone public loos that charge a fee should not be eligible for rate relief; that is not a good way of spending taxpayers’ money. Instead, we propose that owners of fee-charging loos are afforded this choice: either receive relief or continue to charge. They should not be able to do both.
Fee-charging toilets are often privately owned, and fee-charging private toilet facilities in shops, cafés, bars and restaurants have to some degree filled the gap in provision over the past 10 years. The pandemic, however, has exposed the gaping hole in free-to-use public toilets, because a large number of premises with toilet facilities have closed their doors, and people now simply do not carry cash, as shops insist on card payments.
Fourthly, we believe that the Government should publish a report about the impact of the Bill on provision of public lavatories. Throughout the Bill’s passage, it has become apparent that we simply do not have accurate and timely data on how many public loos there are, where they are and how accessible they are; whether they meet the specific needs of parents with young children, people with relevant illnesses or disabilities, women and girls and older people; whether they charge, and who is responsible for maintaining them. It is outside the scope of the Bill and therefore not formally tabled, but we have also asked the Government to consider carrying out an equality impact assessment to assess the decline of public loos.
To summarise, the Bill does provide some relief, so the Opposition will be supporting it. Should the Government reject the amendments that we propose, we would welcome a commitment from the Government to take them away, in the spirit of cross-party working, for consideration in the Lords or outside the Bill process. I remain concerned that in its current form the Bill, though welcome, does not sufficiently remedy the gaps in loo provision. It does not take into account the unprecedented nature of the challenge facing local authorities, nor does it redress the damage done over the last decade.
I believe that the amendments that we have tabled will make the Bill more effective.
Duncan Baker (North Norfolk) (Con)
Bills such as the one before us today may not always be the most high-profile, or garner the most attention, but they make a real difference in our communities up and down the land. Those of us who have “come up through the ranks” by sitting on local councils—in my case Holt Town Council, where I was a rather young-looking mayor in my time—know, from debates, about the annual bone of contention that the running costs of the town’s public loos have become. I am sure that state of affairs is commonplace around the country. But public lavatories are a lifeline. They must be protected, and I warmly commend the Bill for making a difference and doing good in local communities. I am glad that the Opposition do not intend to press amendment 2, because it is important that all loos should be eligible for 100% rates relief, to help all our communities.
Local councils and communities are facing ever-growing pressures and the opportunity to save some public money and shut loos is all too tempting. The Bill will go a long way towards removing a cost and preserving those valuable assets in many of our towns and villages. In my view, access to a lavatory is not just a nicety; it is a fundamental, basic human right.
In North Norfolk, we discovered just how important the public lavatories were when the pandemic set in. My mailbag was full of letters from people in uproar at not being able to use lavatories when they visited the coastal region. That led to all manner of issues; even bus drivers, taxi drivers and delivery drivers could not use those facilities, vital as they were. In coastal communities, where footfall is high owing to the number of our tourist visitors, where there is an ageing demographic and where there are many people with disabilities, lavatories are not just nice to have—they are a basic necessity.
The Bill, for my North Norfolk District Council, will result in a very welcome saving of approximately £80,000 per annum, which is a lifeline for those councils recovering from covid-19. We have one of the most generous provisions in the country: 39 public conveniences, with annual running costs of around £700,000. Those facilities are a vital part of the visitor economy and the Government’s exempting them from business rates is a welcome saving for the authority—part of the package of measures that has been put in place.
Many of my constituents know that I have spent the summer touring my home, mainly along those coastal areas and villages, and can vouch with some first-hand experience that we have the finest public conveniences in the country. There can be few better places in North Norfolk than Cromer’s public lavatories, found on the pier or at the town’s Deep History Coast discovery centre. Alternatively, for those caught short in Blakeney, the Blakeney harbour toilets take some beating for their outstanding location. For those who want something a little different, however, why not take a trip to Walcott seafront to see the new beach and loos, refurbished as part of a £19 million sand-scaping scheme that has delivered a new beach and protected the community?
Before I end, I cannot leave out the work of our parish councils either, especially one of the crown jewels of the North Norfolk coast: Cley next the Sea. The parish council has recently opened its very own public loo, named the Curloo—ornithologists present will understand why the Curloo is so aptly named on my coast. The inspiration for the initiative came from the outstanding parish chair, Dr Victoria Holliday, who led the fundraising project to raise £36,000 in donations to build this invaluable amenity.
There is no greater example of the importance of helping our communities to retain or lower the cost of their public lavatories than Cley Parish Council’s work when Dr Holliday realised that visitors were bypassing the village because those with certain conditions were not coming into the village because of the lack of facilities. Using local trades, the council raised the money to build its very own Curloo. The Bill may be a lifeline for them in saving rates and safeguarding their facilities. The council in Cley can now safely say it will have to fund a little less to have a pee in Cley next the Sea.
I commend the Bill to the House.
Mr Richard Holden (North West Durham) (Con)
I will try to be brief, although I must make a declaration as co-chair of the all-party group on local democracy, which has been pushing for this legislation for some time.
I pay tribute to my hon. Friends the Members for North Cornwall (Scott Mann), for St Austell and Newquay (Steve Double) and for South East Cornwall (Mrs Murray), who have worked on this with me. I would also like to pick up on some of the points made by my hon. Friend the Member for North Norfolk (Duncan Baker), who recognised the great work that his parish councils are doing to keep their public loos going, and to recognise some of my own, some of which I also used on my summer surgery tour this year, in Rookhope, which is run by Stanhope Parish Council and Durham County Council, and in Wolsingham, run by the parish council there. The latter council is one of the reasons why I have been such an active campaigner on this issue, because it is paying about 2% of its annual budget on the rates for the public loos, so this relief today will make a major contribution.
I want to pick up on a couple of the Opposition’s amendments. I am glad they have withdrawn amendment 1, which would have extended the scope of the Bill, and amendment 2, which would have limited it, as they were somewhat contradictory. Amendment 3 would add a level of complexity for much larger councils and is unnecessary at this stage, although it will be well worth considering the issues it raises for inclusion in future legislation.
The Minister of State, Ministry of Housing, Communities and Local Government (Mr Simon Clarke)
Today’s debate has raised some interesting and valid points that help us to understand how the provisions of the Bill will operate. But before I get to the detail of the amendments, let me first remind the Committee of the purpose of the Bill.
As has been discussed, the importance of public lavatories to our communities and economy is recognised by local and central Government alike. In particular, we recognise, especially at this time, the need for access to high-quality facilities to maintain high standards of public hygiene. More broadly, good toilet provision helps the high street and supports the independence of people who rely on those facilities. This small but important measure supports the Government’s strategy to open up our economy and society as we recover from coronavirus and delivers on the Budget 2020 commitment to provide a mandatory business rates relief for public lavatories.
As Members would expect, the Bill has been welcomed by councils that operate public lavatories, as well as by the public who use them. It will ensure that eligible public lavatories, both privately and publicly run, will receive a 100% reduction in their business rates. Crucially, in cutting the costs of public lavatories, particularly in cases in which rates bills make up a significant proportion of their running costs, the Bill will help to keep these vital facilities open.
To ensure that both local authority and privately run facilities receive support to respond to the current pressures, the Bill contains provisions for it to apply with retrospective effect from 1 April 2020. That means that the relief will be backdated to the start of the current financial year. By making the relief mandatory, the full cost of the measure will be met by central Government. Authorities in England will be fully compensated for awarding the relief through the usual grant process. Business rates are, of course, a devolved matter; nevertheless, I am pleased to say that, with the consent of the Welsh Government, the Bill will apply to both England and Wales.
The legislation is needed because all non-domestic properties, publicly or privately owned, are liable for business rates unless they have been specifically exempted from the liability. Public lavatories are not currently excluded from the rates. Although a non-statutory discretionary relief could provide support for privately owned public lavatories, primary legislation is needed to allow local authorities to award relief to the toilets that they run, because legislation currently prevents them from awarding discretionary relief to themselves. I hope the Committee will agree that the Bill is a positive and important measure that will provide critical support to those who run public lavatories.
Let me turn to the amendments, which focus on the scope of the relief. They explore matters such as whether the relief should be awarded to other properties used for wider purposes and whether it should be used to encourage free-to-use public toilets. I appreciate the points made today by the Opposition, and we are taking other measures to help local facilities with their rates bill, but in general terms, as I will explain, I do not believe we should depart from the clear and simple terms of the Bill.
Amendment 1 would extend the scope of the mandatory 100% relief to include publicly owned libraries and community centres and all local authority properties that contain free-to-use public lavatories. The Government’s view is that it is right that public bodies should, like other ratepayers, pay rates on the properties they occupy. As I have set out, legislation therefore restricts local authorities from granting discretionary rate relief on the properties that they occupy. The cost of the Bill in England is estimated to be around £6 million; however, the amendment would significantly increase that. To give an example, to extend the support to public libraries alone would see a tenfold increase in the gross cost of the measure, to around £60 million.
The steps that we are taking to introduce 100% relief for public lavatories recognise the particular importance of the facilities, both in public health terms and to help to ensure that people are able to access and use public spaces. The Government’s policy aim, and the purpose of clause 1, is to target the relief so as best to support the provision of public lavatories. In particular, we want to support facilities that exist where there are unlikely to be any other publicly available toilets, or where removing the additional costs of business rates could make a real difference to the ability of councils or others to keep the facilities open.
All that is not to say that we do not recognise that this is a difficult time for local government—we do. The Government understand the impact of covid on the sector and have therefore made £3.7 billion-worth of funding available to support councils during the pandemic. That is un-ring-fenced precisely because we know that local authorities are best placed to determine how to respond to pressures in their local areas. Additionally, we have promised a new scheme to support councils for lost income by providing for council and business rates tax deficits to be repaid over three years instead of one. Furthermore, we have enabled councils to defer £2.6 billion in business rates payments to central Government.
Amendment 2 would limit the relief to apply only to those public lavatories that are free to use, while amendment 3 would apportion relief to public lavatories where they are part of larger hereditaments as a proportion of the overall assessment of the wider property. I understand the Opposition’s concerns about free-to-use public toilets; nevertheless, the purpose of the Bill is to provide targeted support for separately assessed public lavatories—recognising the particular circumstances that they face—and not to draw a distinction between those that charge and those that do not. I see no harm whatsoever in charging a modest fee to support the service and maintenance of public toilets, and neither do I consider that the public think that unacceptable. I therefore do not agree that the relief should exclude those who charge a fee to use facilities. Such a distinction would add complexity and uncertainty to the wider legislation and risk continuing to impose this tax burden on some stand-alone facilities, which might otherwise close.
On amendment 3, Members are correct in saying that publicly available toilets in properties such as shopping malls will, where they are assessed as part of a larger property, fall outside the scope of the Bill. However, unlike stand-alone toilets, we have not seen evidence to suggest that those toilet facilities are specifically at risk of closure due to the business rates bill. Furthermore, the assessment and administration of such an apportionment, as my hon. Friend the Member for North West Durham (Mr Holden) alluded to, would, in practice, be much more complex and, I fear, far out of line with the level of the resulting rate relief.
Currently, lavatories inside other buildings are not typically given a rateable value in their own right within the wider valuation. Instead, the overall value adopted for the shop or library, for example, merely reflects the presence of a toilet. To meet the aim of the amendment, it would therefore be necessary for the Valuation Office Agency to revalue every eligible building, to reassess its overall value and the value of the lavatory specifically as part of that. That would not only be an artificial and notional exercise for the VOA, but many thousands of properties would potentially need to be reassessed, which would divert resources away from other VOA priorities, such as the operation of the business rates appeals system and the 2023 revaluation. I fear that the amendment would fail to meet the objectives of the policy to target support where it is most needed and would not represent good value for the taxpayer. As I have explained, we have more generally provided a great deal of wider support to local government and ratepayers during the current crisis.
Finally, new clause 1 would require the Secretary of State to conduct and publish an assessment of the impact of this Bill on the provision of public lavatories one year after enactment. I understand that Members will be interested to know what difference this legislation has made over the coming years, particularly given the significant public interest in this issue. I would like to reassure the Committee that the Government keep under review the effectiveness of all the business rates reliefs that we provide. As I have set out, the aim of the Bill is to provide targeted support to those separately assessed toilets to help local authorities keep them open.
Local authorities are ultimately responsible for the provision of public lavatories in their area, and the decision to open or close facilities must rest with them. Nevertheless, the Government strongly encourage councils to keep these facilities open. I recognise the good work of many of our local authorities, some of which we have heard reference to today, in setting up their own community toilet schemes. For example, the London Borough of Kingston has increased provision in its area.
The requirement for there to be a review only one year after the relief comes into force probably would not assist the long-term implementation of the policy. It would not provide enough time to see the true impact of the changes on planning decisions by local authorities or by private companies. As this is a matter for local plans and potentially construction work, it will be many years before the full effect is felt. In the short term, it will be next to impossible to attribute changes in the number of lavatories to this relief or, indeed, to other changes. For example, if more lavatories open, it could be due to the relief, or it could be due to a wider tourism boom in coastal areas such as North Norfolk. Simply looking at changes in the number of lavatories will therefore not necessarily be a good measure of the impact of the relief. Nevertheless, I assure the Committee that we will continue to keep all reliefs, not just this one, under review, together with my colleagues in the Treasury, as part of its wider review of business rates.
I am grateful to the hon. Member for Blackburn (Kate Hollern) for not pressing her amendments to a vote. This is a good Bill that will make a real difference to the lives of many people, and I commend it to the House.
Kate Hollern
I beg to ask leave to withdraw the amendment.
Amendment, by leave, withdrawn.
Clauses 1 to 4 ordered to stand part of the Bill.
The Deputy Speaker resumed the Chair.
Bill reported, without amendment.
Third Reading
Mr Simon Clarke
I beg to move, That the Bill be now read the Third time.
This Government know how important good lavatory provision is for all of us at work, in our leisure time or as we shop, and this Bill delivers on the commitment made by the Government at Budget to establish a 100% mandatory business rate relief for eligible public lavatories.
I would like to take this opportunity to thank Members on both sides of the House for their positive contributions, in particular my hon. Friends the Members for North Norfolk (Duncan Baker) and for North West Durham. This Bill has genuine cross-party support, and I am grateful to the hon. Member for Blackburn for her constructive comments. I am also grateful to those who, on Second Reading, fully supported this measure, particularly my hon. Friends the Members for St Austell and Newquay (Steve Double) and for North Cornwall (Scott Mann), who have both worked tirelessly in support of getting this measure on to the statute book. This represents mission accomplished. Furthermore, I would like to reiterate the welcome support offered to the Bill’s passage from the National Association of Local Councils and the British Toilet Association, as well as local authorities, including town and parish councils up and down our country, who have worked so hard to open their facilities to the public and to support their local communities.
During the passage of the Bill, a number of questions and points have been raised that it may be helpful for me to address briefly. I can confirm that local authorities will be fully compensated by central Government for awarding the relief, including those lavatories run by parish and town councils. Subject to enactment of the Bill, the relief will apply with effect from 1 April this year, meaning that eligible properties will receive a backdated discount, ensuring that they will pay nothing in the current financial year and onwards. In line with other reliefs, local authorities will be responsible for determining eligibility within the scope of the legislation and will award support to those lavatories that they consider to qualify for support.
It is also worth noting that in late July, the Government published our response to the Changing Places consultation and announced changes to building regulation guidance to mandate the provision of Changing Places toilets for the most severely disabled in many new public buildings. That is the right thing to have done and it is something that we can all be proud of across the House.
This Bill is a positive measure, which has been widely welcomed by those who run public lavatories, and provides support to help keep these facilities open. I commend it to the House.
Kate Hollern
I will keep this brief, as I am sure the Minister will be pleased to hear. It is disappointing that the Government have rejected our amendments, which, for reasons already outlined, we believe would have further widened public access to loos. The Minister will be aware that there are strong feelings in both Houses about the number, quality and accessibility of public loos, and the Lords will return to the matters that we have raised in our amendments.
The Bill as it stands is a welcome attempt to cover some of the costs associated with public lavatories, and for that reason, we will support it. The relief that the Bill provides does not cover all the costs of maintaining public loos, given the enhanced cleaning regimes that councils and other loo providers have put in place to tackle covid.
I sincerely hope that introducing the Bill at this time is a signal from the Government that they are committed to supporting councils, many of which have run public toilets during this crisis. If the Government are serious about saving public loos, they should also consider our request to carry out an equality impact assessment. Doing so would be a tangible demonstration that the Government are committed to supporting the most vulnerable.
Question put and agreed to.
Bill accordingly read the Third time and passed.
This Bill should now be sent for Royal Ascent by the Queen and it will then become an ACT of Parliament and enter into Law.
The following LINK will direct you to and allow you to view the full Hansard Report from Westminster
Social distancing and making your workplace COVID-secure

Including Bathrooms, Toilets and Washbasins
Social distancing means keeping people apart to help reduce the spread of coronavirus.
Where possible you should keep people 2m apart. If this is not viable, keeping 1m apart with risk mitigation is acceptable.
In the UK some rules such as social distancing may be different in each of the devolved nations. However, HSE regulates in all of these countries. You should check the public health guidance for the country you are in:
You must ensure that workers and other people visiting your workplace understand and comply with the measures you put in place.
Social distancing should form part of your business’s risk assessment and is one of the steps needed to make your workplace COVID-secure.
The gov.uk guides on working safely during coronavirus (COVID-19) explain the control measures that different types of business should consider. These cover construction, factories, offices, vehicle use and other types of work. The guides apply to workplaces in England.
The following guidance sets out the main control measures and additional measures where social distancing is not possible:
- Common areas (includes break areas, bathrooms, toilets, meeting rooms and accommodation)
- Workstations
- Arriving and leaving work
- Movement around buildings and worksites
- Where 2m social distancing is not possible
- Using vehicles
- Emergencies, security and other incidents
Common areas (includes break areas, bathrooms, toilets, meeting rooms and accommodation)
Common areas are used by many people. The potential for spread of coronavirus is considered to be higher in these areas if proper controls are not in place.
Identify and review the common areas within your workplace including:
- restrooms
- kitchens
- tea points
- changing facilities
- lifts
- meeting rooms
- smoking areas
- canteens
- toilets
- showers
- reception areas
- accommodation
Also consider pinch points in your premises such as narrow corridors, staircases, doorways and storage areas.
You may need to put in place a combination of control measures to keep people safe.
General control measures
Consider putting the following control measures in place for common areas:
- Limit the number of people at any one time using any areas that may become congested.
- Use floor markings to maintain social distancing.
- Keep surfaces clear so that cleaning can be carried out more effectively.
- Identify objects that may be touched more frequently, such as kettles, cooking equipment, phones, computers or tables and make sure that they are frequently cleaned.
- Try to maximise ventilation.
- Make sure that your workforce is clear on the rules when using common areas.
- The areas should be regularly cleaned in line with your cleaning plan.
- Minimise contact between people, using barriers or screens.
- Provide hand-washing facilities or hand sanitiser near to frequently used areas.
- Display signs reminding people to socially distance, wash hands and not touch their faces.
- Work with landlords and other tenants in multi-tenant sites or buildings to ensure consistency across areas such as receptions and staircases.
Guidance on cleaning, hygiene and hand sanitiser.
Break areas
Employers must make sure all workers, including those visiting your premises for work, have somewhere to rest and eat and should also provide facilities to heat food or water for hot drinks. Find out more about having the right workplace facilities.
Consider these control measures:
- Ensure that workers understand the need to maintain social distancing and good hand hygiene before entering any areas where food is consumed.
- If workers need to leave the site at break times remind them to maintain social distancing while off-site.
- If canteens are used, consider if food, cutlery etc can be delivered to tables. Where canteens need to serve food reconfigure seating and tables to maintain spacing and reduce face-to-face interactions. Mark the floor in case furniture is accidentally moved.
- Stagger or extend break times to limit the numbers of people using the facilities.
- Create additional break areas where required such as in unused rooms. It may be possible to create outside break areas where it is safe to do so.
Bathrooms, toilets and washbasins (welfare facilities)
You have a legal duty to provide adequate toilet and washing facilities that are easy and safe to access. This applies to any workers (including those not employed or contracted to you), and visiting workers who are not normally on your premises. The legal responsibility to provide access to these facilities lies with whoever controls the premises.
Refusing access for any reason, including as an infection control measure, is against the law. It is vital that people can wash their hands regularly, so not allowing access to welfare facilities may increase the risk of COVID-19 spreading.
When completing your COVID-19 risk assessment, review the provisions you have to make sure they allow people (including visiting workers) to social distance, use the toilets and wash hands frequently. Consider whether you need to provide any additional washing facilities.
To protect people when using existing toilet and washing facilities consider the following:
- Identify all surfaces that require additional cleaning in bathrooms and toilets.
- Taking some static facilities out of use where they are less than 2m apart. If this includes toilet facilities such as urinals you should ensure that you still have a sufficient number of toilets in your workplace.
- Put markings on floors to show people the right distances or where to stand.
- Put in place systems such as ‘one in, one out’ if it isn’t possible to maintain social distancing.
- Make sure you provide running water and soap to enable people to clean their hands properly.
- Provide hand drying facilities – paper towels or hand dryers.
- Empty bins frequently to safely dispose of waste. Where possible have open-topped bins or foot operated lids.
- Using signs and posters to increase awareness of good handwashing technique.
- Decide how and when handwashing facilities will be cleaned and when bins will be emptied.
- Decide who will replenish soap, paper towels and hand sanitiser.
Guidance on cleaning, hygiene and hand sanitiser.
Additional handwashing facilities
When completing your COVID-19 risk assessment, consider if you need to provide additional handwashing facilities so that people can wash their hands frequently.
Consider:
- where people work
- how much contact they have with others
- the frequency they should wash their hands as a result
This will also help you to decide if and where you need to provide additional washing facilities.
If you cannot provide additional handwashing facilities, you may need to provide hand sanitiser instead in some circumstances.
When you complete your risk assessment, think about:
- providing handwashing facilities at entry and exit points so people can wash their hands when they arrive and leave work – if this is not possible, provide hand sanitiser
- where extra handwashing facilities need to be to allow people to wash their hands frequently
- making sure your handwashing facilities have running water, soap and paper towels or hand dryers
- identifying where extra hand sanitiser points are needed in addition to washing facilities
Meeting rooms
Consider the following measures:
- Use remote working tools to avoid in-person meetings.
- That only absolutely necessary participants should physically attend meetings and should social distance throughout.
- Avoid sharing pens, documents and other objects.
- Provide hand sanitiser in meeting rooms.
- Hold meetings outdoors or in well-ventilated rooms whenever possible.
- For areas where regular meetings take place, using floor markings to help people maintain social distancing.
Accommodation
Employers who provide accommodation for their workers should consider the following:
- Identify measures to keep workers safe while they are staying in accommodation and working, in your risk assessment.
- Minimise numbers of people living in shared accommodation.
- Treat each accommodation living unit (eg caravan) as a ‘household’.
- How you will ensure if one person in the ‘household’ shows symptoms that all will self-isolate in line with the guidance for households with possible coronavirus infection.
- Workers should not live or stay in more than one ‘household’.
- Keep people who live in the same household together in the same work group.
- Try not to mix households while they are working.
- Try to keep each household socially distanced from other households.
- Check workers health before they start work each day.
- If a worker develops symptoms of coronavirus while working they should return to their household. The individual, and anyone else highlighted by government guidance should then follow the government guidelines on isolation.
- Cleaning regimes to ensure accommodation units stay clean.
- Cleaning regimes for shared communal areas. The employer is responsible for making sure that communal areas are properly and regularly cleaned.
- Carryout statutory checks such as landlord gas safety checks as required.
- Cleaning and maintenance regimes for toilets and showers.
- Provide fire safety precautions as normal.
Workstations
Workstations are areas where workers routinely or regularly work and can include:
- desks or tables in the workplace
- production or processing lines
- areas by machinery that workers need to operate
- desks within workers homes if they are working at home
- vehicles
Consider the following:
- Look at how you can organise workstations to allow people to meet social distancing rules.
- Review layouts and processes to allow people to work 2m apart from each other where possible.
- Use floor tape or paint to mark areas.
- Manage occupancy levels.
- Avoid any sharing of workstations, including hot desking where possible.
- Limit the number of people having to share a workstation to the absolute minimum.
- Where workstations must be shared, try to keep the same set of people using them.
- Make sure that workstations are cleared at the end of the day or shift so that they can be properly cleaned.
- Ensure that all workstations are regularly cleaned in accordance with your cleaning plan.
Where it’s not possible to keep workstations 2m apart, consider these additional control measures.
Guidance on cleaning, hygiene and hand sanitiser.
Arriving and leaving work
Consider these control measures for when people are arriving or leaving work:
- Take precautions to limit the chances of anyone with coronavirus entering your premises, for example, display signs asking people not to enter your workplace if they have symptoms of coronavirus.
- Limit the number of people entering your workplace, or parts of your workplace, to avoid overcrowding. Think about if you can you arrange partial working from home for some staff.
- Stagger arrival and departure times to reduce crowding into and out of the workplace, taking account of the impact on those with protected characteristics.
- Provide additional parking or facilities such as bike racks to help people walk, run, or cycle to work where possible.
- Provide more entry points to reduce congestion.
- Provide more storage for workers for clothes and bags. Encourage storage of personal items and clothing in personal storage spaces, for example lockers during shifts.
- Use markings and introduce one-way flow at entry and exit points.
- Provide handwashing facilities at entry and exit points, or hand sanitiser where handwashing is not possible. Make sure you provide these facilities for anyone entering your workplace.
- Where possible, avoid using touch-based security devices such as keypads. If you need to use them, make sure they’re cleaned regularly.
- Where possible, introduce shift working to limit the number of people in the workplace at any one time. This may also reduce the burden on public transport if your employees use it to travel to work.
- Where possible, introduce suitable barriers or screens where people regularly interact, such as service desks or reception areas. If used, ensure they are cleaned and disinfected in line with your cleaning procedures.
- Put in place procedures for dealing with deliveries and visitors. Allocate time slots for customers.
- Put in place measures to keep delivery drivers safe, this includes allowing delivery drivers to use welfare facilities.
Guidance on cleaning, hygiene and hand sanitiser.
Movement around buildings and worksites
Consider these control measures when people are moving around buildings or worksites:
- Use floor markings to mark out social distancing. Focus particularly on the most crowded areas, for example where queues form, entry points to buildings, toilets and communal break areas. Additional control measures may be needed for areas at higher risk of overcrowding, such as common areas.
- Use any unused spaces to allow people to spread out and comply with social distancing rules.
- Reduce movement by discouraging non-essential trips within buildings and sites, for example restricting access to some areas, encouraging use of radios or telephones or other electronic devices, where permitted, and cleaning them between use.
- Restrict access between different areas of a building or site.
- Reduce job and location rotation.
- Introduce more one-way flow through buildings.
- Reduce maximum occupancy for lifts. Provide hand sanitiser for the operation of lifts. Encouraging use of stairs wherever possible.
- Make sure that people with disabilities are able to access lifts.
- Manage the use of high-traffic common areas including corridors, lifts turnstiles and walkways.
- Put in place measures to remind staff and visitors to follow social distancing.
Where 2m social distancing is not possible
Consider these additional control measures where 2m social distancing is not possible:
- Consider if the activity needs to continue or if it can stop.
- Keep the number of people working who cannot social distance to a minimum.
- Reduce the number of people in close proximity in the work area.
- Limit the movement of people around the site. Consider if workers stay in one place, or at one workstation when working.
- Limit the amount of different equipment or surfaces that people need to touch.
- Assign workers to teams which then socially distance from other teams. Keep workers in the same teams as far as possible to limit social interaction. Keep teams as small as possible. If a team member becomes ill with symptoms of coronavirus, they and the rest of the team should follow the UK government guidance on self-isolation.
- Use screens between people to create a physical barrier. You should keep the screens clean.
- Organise the space so that people are side-by-side or facing away from each other rather than face-to-face.
- Mark the floor of areas such as lifts to show where people should stand and what direction they should face.
Guidance on cleaning, hygiene and hand sanitiser.
Using vehicles
On gov.uk there is guidance for people who work in or from vehicles setting out control measures to help protect workers.
Consider the following control measures:
- If travel in vehicles is needed for the business to continue to operate.
- Ensure those who are travelling are necessary for the work to be carried out.
- Limit passengers in corporate vehicles such as work minibuses. This could include leaving seats empty.
- Consider if social distancing measures can be implemented in the vehicle.
- Avoid multi-occupancy vehicles where safe to do so.
- Where multi-occupancy vehicles are used, people should social distance where possible through suitable seating arrangements and where necessary, use of additional transport. Keep the journey as short as possible.
- Where more than one person is travelling and they need an overnight stop, plan ahead to ensure there is suitable accommodation secured to ensure social distancing.
- Consider if people who need to travel in vehicles can be kept in the same teams.
- Consider if vehicle windows can be kept open.
- Ensure that people practice good hygiene before and after using the vehicle. Provide hand sanitiser where necessary.
- Vehicles should not be shared between different users if possible.
- Remind workers to travel alone to and from work where possible, either in their own transport, by walking, or cycle if it is safe to do so.
- Ensure vehicles are cleaned regularly, in particular between different users. Clean commonly touched areas in vehicles including:
- handles (inside and out)
- steering wheel and starter button
- centre touchscreen and stereo
- handbrake and gearstick
- keys and key fob
- indicators and wiper stalks
- windows, mirrors and mirror switches, seat adjusters any other controls
Where it’s not possible for people to social distance in a vehicle, consider additional measures such as:
- using physical screening, as long as this does not compromise safety, for example by reducing visibility
- sitting side-by-side not face-to-face
- using a fixed pairing system if people have to work in close proximity
Drivers’ welfare at delivery and collection sites during the coronavirus (COVID-19) outbreak
Emergencies, security and other incidents
Consider the following:
- Reviewing your incident, first aid and emergency procedures to ensure people can social distance as far as possible.
- Considering the security implications of any changes you intend to make to your operations and practices in response to the coronavirus outbreak as any revisions may present new or altered security risks.
- For organisations who conduct physical searches of people, considering how to ensure safety of those conducting searches while maintaining security standards.
CORONAVIRUS, SARS-COV-2, COVID-19 AND HVAC SYSTEMS

This response outlines the current understanding of the possible routes of transmission of the SARS-CoV-2 virus (including airborne aerosol transmission) and possible responses that Building Services Engineers can adopt to reduce transmission risks in the built environment.
The current coronavirus (COVID-19) outbreak continues to develop rapidly with relevant advice being updated regularly and an increasing body of research being published.
Government, NHS and Public Health England websites, as well as those of the devolved administrations should be consulted for current policy across the UK.
CIBSE is the UK member of REHVA, the European Federation of Heating and Ventilation Engineers. REHVA has developed a COVID-19 guidance webpage giving information and guidance and has developed a bibliography on how to operate and use building services to minimise the spread of the virus through HVAC or plumbing systems. The guidance was further updated on 3rd April 2020 to reflect new knowledge and evidence becoming available.
Current Public Health England guidance on infection control states that “The transmission of COVID-19 is thought to occur mainly through respiratory droplets generated by coughing and sneezing, and through contact with contaminated surfaces. The predominant modes of transmission are assumed to be droplet and contact.” (See section 2.1 of the guide).
Droplets will generally fall out of the airstream within a short distance (depending on airflow speed and direction), hence the guidance to remain 2m apart. However, these may evaporate, reducing in size and mass and travel further in air streams, contaminating surfaces and increasing the risk of airborne transmission.
While airborne transmission is not thought to be a primary route of transmission, there is an emerging and growing body of evidence that the SARS-CoV-2 can also be spread through the air, particularly in poorly ventilated indoor spaces, and that ventilation provision in buildings should be reviewed in the light of this. For an explanation of airborne transmission, see the series of tweets by Prof. Lynsey Marr.
Emerging Findings
Proving modes of transmission during an outbreak is difficult. However, multiple recent studies are showing evidence of indirect contact (which may be linked to airborne spread) and have also linked airflow patterns to infection cases.
This has been particularly the case in high occupancy areas, in spaces with little outdoor air, and when people generate a lot of aerosols (e.g. shouting and singing). Given the growing body of evidence suggesting airborne transmission may be a route of infection and knowledge of aerosol generation and transport it is prudent to ensure ventilation is operating appropriately to protect occupants.
The following measures, using outside air wherever possible, should help to reduce the risks from airborne transmission.
Prevention
The primary mechanisms for preventing the transmission of coronavirus remain regular, thorough handwashing using soap and hot water for at least 20 seconds, coupled with strict adherence to social distancing requirements and staying at home. Surfaces which may be contaminated also need regular cleaning following the protocols set out by PHE.
Dilution of internal air should reduce any risk of potential airborne viral transmission by reducing exposure time to any airborne viral aerosols, and also reduce the chance for these aerosols to settle on surfaces. Evidence shows that virus can survive on some surfaces for at least 72 hours and hence any action to limit surface contamination is beneficial.
It is recommended that any ventilation or air conditioning system that normally runs with a recirculation mode should now be set up to run on full outside air where this is possible.
In buildings with mechanical ventilation systems extended operation times are recommended. In demand control systems CO2 set points should be set to 400ppm to increase the delivery of outside air. Ventilation should be kept on for longer, with lower ventilation rates when people are absent. It is not recommended to switch ventilation systems off in any buildings, even those temporarily vacated, but to operate them continuously at reduced speeds.
Recirculation of air between spaces, rooms or zones occupied by different people should be avoided. However, in the case of any systems serving a single space, partial recirculation of air within that space, such as through a local fan coil unit, is less of a concern. The reason is that the primary objective is to maximise the air exchange rate with outside air and to minimize the risk of any pockets of stagnant air.
If a local recirculation unit enhances air disturbance and hence helps reduce the risk of stagnant air then this should be considered when developing a strategy. Note that although these are relatively uncommon today, ceiling fans within a space can provide this function.
On colder days consideration must be given to human behavioural responses. A ventilation system on full outside air which is not adequately heated may create discomfort draughts. This may lead to users seeking to turn the system off, or with naturally ventilated spaces users may close vents or windows. These actions will reduce the air exchange rate and dilution of any contaminants (and not just any viral contamination) and overcome the primary objective of the ventilation strategy. It is important that where users can intervene in the control of the ventilation that they are made aware of the benefit of these for reducing the circulation of infectious material.
Care should be taken with any ventilation grills that can be blocked, e.g. floor grilles for displacement ventilation, and occupants educated on the purpose and benefits of these.
The potential benefit to public health at this time outweighs the reduction in energy efficiency caused by not recirculating air. Airborne contaminants may be minimised by proper and effective filtration and regular maintenance. Viral material that settles in ductwork will become unviable over time. In the event that some viral material entered ventilation and air-conditioning systems prior to buildings being vacated due to the current restrictions, it is extremely unlikely that that material will pose any risk when those buildings are re-occupied.
Where cleaning or planned maintenance of ventilation systems is required, such as in catering premises, it should be undertaken in line with agreed industry guidance, including that relating to site operations under social distancing requirements. Appropriate PPE should be worn and all materials, including old filters, should be carefully bagged and disposed of safely. Given the requirement for many business premises to close for the immediate future, there is unlikely to be a requirement to undertake work on their ventilation or air conditioning systems at this time.
In poorly ventilated spaces with a high occupancy and where it is difficult to increase ventilation rates it may be appropriate to consider using air cleaning and disinfection devices. The most appropriate devices are likely to be local HEPA filtration units or those that use germicidal UV (GUV) radiation. GUV devices use radiation in the UV-C spectrum and have been shown to inactivate coronaviruses, although there is not yet specific evidence of the efficacy of UV-C irradiation for SARS-CoV-2.
There are currently uncertainties about a variety of factors affecting UV performance including dosage, wavelength and exposure time. In addition, consideration will need to address the specific room and system configuration, air flow, distribution and humidity.
Any potential equipment will need to be properly tested, validated and quality assured and demonstrated to provide the specific irradiation properties it is designed to and nothing else. It is essential that appropriate safety interlocks are installed to ensure UV cleaning equipment is not operated when people may be exposed to the radiation.
They can be applied as an upper-room system or a stand alone consumer unit, but it is important that these are sized correctly for the room as many do not have the flow rate to be effective in larger spaces. In-duct UV-C is not recommended to control disease transmission unless it is to decontaminate air that is recirculated. Devices that emit ozone or other potentially hazardous by-products should not be used in occupied spaces. Further guidance on air cleaning and disinfection is given in CIBSE guide A.
Further Guidance
CIBSE TM40 Health and Wellbeing in Building Services provides guidance on best practice design and operation of buildings to support health, comfort and cognitive performance. Key aspects covered include air and water quality and the environment around us: light, acoustics, thermal and humidity conditions, and electromagnetic fields. The health and comfort impact of each of these environmental factors is summarised to provide a background for informed decisions.
The April 2020 issue of CIBSE Journal carries news and opinion on COVID 19, and there is a CIBSE Journal podcast which addresses the issues in further detail.
The REHVA COVID-19 guidance webpage provides further information and guidance and a bibliography on how to operate and use building services to minimise the spread of the virus through HVAC or plumbing systems.
References
The following references inform the emerging view that aerosol transmission of SARS-CoV-2, whether through direct respiratory droplet transfer or fomite generation, may in fact be a more important exposure transmission pathway than previously considered. Many are still undergoing peer-review, but they demonstrate the current thinking based on emerging findings.
Fears et al, Comparative dynamic aerosol efficiencies of three emergent
coronaviruses and the unusual persistence of SARS-CoV-2 in aerosol
suspensions https://www.medrxiv.org/content/10.1101/2020.04.13.20063784v1.full.pdf
https://doi.org/10.1101/2020.04.13.20063784
PREPRINT posted 18th April 2020
van Doremalen, N et al Aerosol and Surface Stability of SARS-CoV-2 as Compared
with SARS-CoV-1. New England Journal of Medicine 2020 doi
10.1056/NEJMc2004973 https://www.nejm.org/doi/full/10.1056/NEJMc2004973
This letter was published on March 17, 2020, at NEJM.org.
Fineberg: Rapid Expert Consultation on the Possibility of Bioaerosol Spread of
SARS-CoV-2 for the COVID-19 Pandemic (April 1, 2020) (2020) https://www.nap.edu/read/25769/chapter/1
Letter in response to the consultation.
Lidia Morawska, Junji Cao, Airborne transmission of SARS-CoV-2: The world
should face the reality, Environment International, Volume
139,2020,105730,
https://doi.org/10.1016/j.envint.2020.105730.
This is a preprint of a paper for publication in the June issue
Yuguo Li et al : Evidence for probable aerosol transmission of SARS-CoV-2 in a poorly ventilated restaurant https://www.medrxiv.org/content/10.1101/2020.04.16.20067728v1.full.pdf Preprint posted 22 April 2020
The Chartered Institution of
Building Services Engineers (CIBSE)
Registered as a Charity in England No. 278104
HSE Guidance on Ventilation and Air Conditioning systems

Air conditioning and ventilation during the coronavirus outbreak:
Received in Septemeber 2020
This guidance is based on the latest information and may be updated as and when new information becomes available.
General ventilation
Employers must, by law, ensure an adequate supply of fresh air in the workplace and this has not changed.
Good ventilation can help reduce the risk of spreading coronavirus, so focus on improving general ventilation, preferably through fresh air or mechanical systems.
Where possible, consider ways to maintain and increase the supply of fresh air, for example, by opening windows and doors (unless fire doors).
Also consider if you can improve the circulation of outside air and prevent pockets of stagnant air in occupied spaces. You can do this by using ceiling fans or desk fans for example, provided good ventilation is maintained.
The risk of transmission through the use of ceiling and desk fans is extremely low providing there is good ventilation in the area it is being used, preferably provided by fresh air.
Air conditioning
The risk of air conditioning spreading coronaviru s (COVID-19) in the workplace is extremely low as long as there is an adequate supply of fresh air and ventilation.
You can continue using most types of air conditioning system as normal. But, if you use a centralised ventilations system that removes and circulates air to different rooms it is recommended that you turn off recirculation and use a fresh air supply.
You do not need to adjust air conditioning systems that mix some of the extracted air with fresh air and return it to the room as this increases the fresh air ventilation rate. Also, you do not need to adjust systems in individual rooms or portable units as these operate on 100% recirculation. You should still however maintain a good supply of fresh air ventilation in the room.
If you’re unsure, ask the advice of your heating ventilation and air conditioning (HVAC) engineer or adviser.
Ventilation
General ventilation
- All workplaces need an adequate supply of fresh air
- This can be natural ventilation, from doors, windows etc or controlled, where air is supplied and/or removed by a powered fan
- If you work in an office or shop, natural ventilation will normally be enough to control dusts and vapours from cleaning materials etc
- Sometimes planned, powered general ventilation is an integral part of a set of control measures, eg the welding of large fabrications in a workshop
Local exhaust ventilation
- Local exhaust ventilation (LEV), or extraction, is an engineering control solution to reduce exposures to dust, mist, fume, vapour or gas in a workplace
- Use a properly designed LEV system that will draw dust, fume, gases or vapour through a hood or booth away from the worker
- An extraction system should be easy for workers to use and enclose the process as much as possible
- It should effectively capture and contain the harmful substance before it is released into the working environment
- Air should be filtered and discharged to a safe place
- The system should be robust enough to withstand the process and work environment. It is important to maintain it and undertake tests to ensure it is working effectively
Things to avoid when applying LEV
Common errors in applying extraction are:
- the effectiveness of small hoods is usually overestimated – be realistic
- the hood is usually too far away from the process
- the hood doesn’t surround the process enough
- inadequate airflow
- failure to check that the extraction continues to work
- workers are not consulted, so they don’t understand the importance of extraction and do not use it properly
How a local business woman adopted a closed toilet block

Chloe Pavely decided the council’s closure of a toilet block near her cafe in Brixham, Devon, was a minor inconvenience.

So she adopted it and thanks to support from locals the toilet is still giving relief to passers-by at Fishcombe Cove.
‘Living the dream and that includes looking after the toilet block’
The toilet was one of three closed this year by Torbay Council which said it was spending £2m upgrading others in the area.
The BTA board has acknowledged this fantastic commitment and is considering awarding Chloe a special certificate of thanks and appreciation of the efforts that she is making to help residents and visitors to find much needed comfort and relief whilst enjoying Fishcombe Cove.

CoronaVirus: a report on Warm Air Dryers & Paper Towels

Airdri: paper – Microbiologist’s report
As an experienced microbiologist, I have been asked if I feel safe using a public washroom in the current coronavirus pandemic and how the virus could be transmitted in a washroom? The virus responsible for the pandemic has been named ‘severe acute respiratory syndrome coronavirus 2’ (or SARS-CoV-2) and this causes the disease COVID-19.
The second question is easy to answer: Current informed opinion shows that SARS-CoV-2 is spread by droplet transmission, and also by contacting contaminated surfaces and then touching your face. UK Government, NHS, CDC and WHO sources all emphasize social distancing and the need for adequate handwashing as well as hand sanitation to prevent transmission. The risks of contracting COVID-19 should be no greater in a washroom than in any other communal space.

If washroom users have no obvious symptoms of COVID-19 there should be little risk of infection, however there is some debate about the release of SARS-CoV-2 by people before they show symptoms, so there is a possibility of being exposed to contaminated air and surfaces[1]. However the risks are probably greater in the general workplace where coughing and sneezing (and even speaking[2]) can release airborne SARS-CoV-2 which can survive up to 15 minutes in droplets and aerosols in air [3]. With droplet transmission respiratory droplets are generally large enough (> 100 microns in diameter) to fall to the floor rapidly and within 2 meters of the person who is coughing or sneezing.[4] These droplets should adhere to surfaces and the floor as they are comprised of mucus – reducing the risk of transmission. Droplet transmission of coronaviruses by washroom activities is also unlikely as the air is constantly changed, typically 8 – 12 times per hour,[5,6] which will remove droplets as will ‘natural’ ventilation due to opening and closing doors. Many smaller washrooms are also fitted with ‘air purifiers’ to control odours and remove microbial contaminants. Previous (pre-pandemic) studies on the spread of droplets containing faecal bacteria from flushing toilets, operating hand dryers and handwashing have detected faecal bacteria in the air and on surfaces, with Escherichia coli, Streptococcus and Salmonella bacteria being found in public washrooms, and pathogenic Clostridium difficile and MRSA detected in hospital washrooms and toilets.[7,8,9] SARS–CoV-19 has been reported in faeces[10] however there are no reports of transmission via this route.
One notable feature of this research has been the long-standing debate about the relative advantages (or otherwise) of hand dryers over paper towels and their role in the transmission of pathogens. Much of the research is related to hospital usage of hand dryers, and it is generally accepted that they should not be used in clinical areas due to the noise rather than any published epidemiological evidence to show that they are unsafe.
This debate is fueled by the sales of paper towels and hand dryers in the washroom sector: market research indicates that sales of multi-fold paper towels will reach $4bn this year while sales of hand dryers will reach $856m, having grown 12% every year since 2014. The paper towel manufacturers, supported by some biased scientific literature and scaremongering in the public press, report that hand dryers are unhygienic and contribute to the spread of pathogenic bacteria and viruses in the washroom.
In response, the hand dryer industry reports that both paper towels and their dispensers can harbour significant amounts of pathogenic bacteria and viruses, that used towels cannot be recycled and they have a negative environmental impact. [11,12] Potentially pathogenic microbes are spread in the washroom by the users not washing and drying their hands correctly and via the HVAC system supplying contaminated air from other rooms in the building.[13] In a small (50 m3) washroom, a single operation of a typical hand dryer would only disturb 2-3% of the volume of air in a single operation and is unlikely to contribute to the spread of microbes.
The reality is that there is no real difference between paper towels and hand dryers when it comes to cleanliness.[11]
In the light of available information about SARS-CoV-2 and COVID-19 there are two key facts which emerge and warrant attention:
The first, particularly in the present pandemic, is the importance of hand-washing. Most of the hygiene problems arising in washrooms to date have been due to inadequate hand washing. Pre-pandemic observations have shown that nearly 95% of adults did not wash long enough to thoroughly clean bacteria and viruses from their hands.[14]
Furthermore, one UK study reported that:
99% of people visiting a public washroom said they had washed their hands after going to the toilet however, recording devices showed that only 32 percent of men and 64 percent of women actually had.[14] Washing is the key to the removal of bacteria and viruses, and organizations such as the WHO, CDC and DHSS detail the correct way to do it. [15,16,17]
The second is the importance of drying hands properly. In several studies people spent, on average, just 22.5 seconds drying their hands and 45% of washroom users wiped their hands on their clothing to finish drying.[18] An observational study in 2006 timed 5000 hand drying events at a motorway service station and noted that men used the warm air hand dryers for an average of 20 seconds, whilst women used them for just 16 seconds. These reported mean drying times are substantially below 30 seconds, so it can only be concluded that most users of warm air hand dryers do not achieve full drying of their hands. [19]
The World Health Organization has stated that:
“To protect yourself against the new coronavirus, you should frequently clean your hands with an alcohol-based hand rub or wash them with soap and water. Once your hands are cleaned, you should dry them thoroughly by using paper towels or a warm air hand dryer.” [20]
The key message for hand hygiene in washrooms is:
1. ensure the hands are correctly washed,
2. ensure hands are thoroughly dried (10 seconds of drying with either paper towels or jet air dryers; or up to 40 seconds using a warm air hand dryer [21]),
3. do not touch any surfaces after drying hands, and if you do
4. use a hand sanitizer when outside the washroom.
In answer to my first question – “would I feel safe using a public washroom in the current pandemic?” is “yes, it is now probably safer than I did in pre-pandemic days. If people wash their hands correctly, and then dry using either hand towels or hand dryers according to WHO guidelines transient micro-organisms derived from contact will be washed off (soap has been shown to denature SARS-CoV-2),: and any aerosol generated from clean hands by hand dryers will not transmit pathogenic bacteria or viruses into the washroom”.
REFERENCE DOCUMENTS AND WEBSITES
[1] https://www.medrxiv.org/content/10.1101/2020.03.23.20039446v2
[2] https://medicalxpress.com/news/2020-04-important-speech-transmitting-coronavirus.html
[3] https://www.nejm.org/doi/pdf/10.1056/NEJMc2004973
[4] https://onlinelibrary.wiley.com/doi/full/10.1111/j.1600-0668.2009.00626.x
[5] https://www.hse.gov.uk/pUbns/priced/l24.pdf
[6] http://www.solutionsforair.com/resources/rulesofthumb/restroom.aspx
[7] https://www.initial.com/assets/content/files/journey-of-the-germ-white-paper.pdf
[9] https://microbewiki.kenyon.edu/index.php/Microbiology_of_Hospital_Washrooms
[10] https://www.livescience.com/coronavirus-covid-19-spread-through-feces.html?
[11] https://www.theguardian.com/society/2019/apr/25/hand-dryers-paper-towels-hygiene-dyson-airblade
[12]https://www.intelligenthanddryers.com/blog/hand-dryers-are-they-hygienic
[13] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5881072/
[14]https://www.transplumb.com/news-archive/news-2017/16-03-17-srticle-proper-handwashing-and-drying
[15] https://www.who.int/gpsc/clean_hands_protection/en/
[16] https://www.cdc.gov/handwashing/index.html
[17]https://www.nhs.uk/live-well/healthy-body/best-way-to-wash-your-hands/
[18] http://info.debgroup.com/blog/bid/297155/Paper-Towels-or-Hot-Air-Dryers-Which-is-Better-Why
[19] https://sfamjournals.onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2672.2010.04838.x
[21] http://www.nhs.uk/news/2013/06June/Pages/Paper-towels-may-be-more-hygienic-than-hand-dryers.aspx
Dr. David L. Webber 10th April 2020
Related products: NEW Air Purification Units
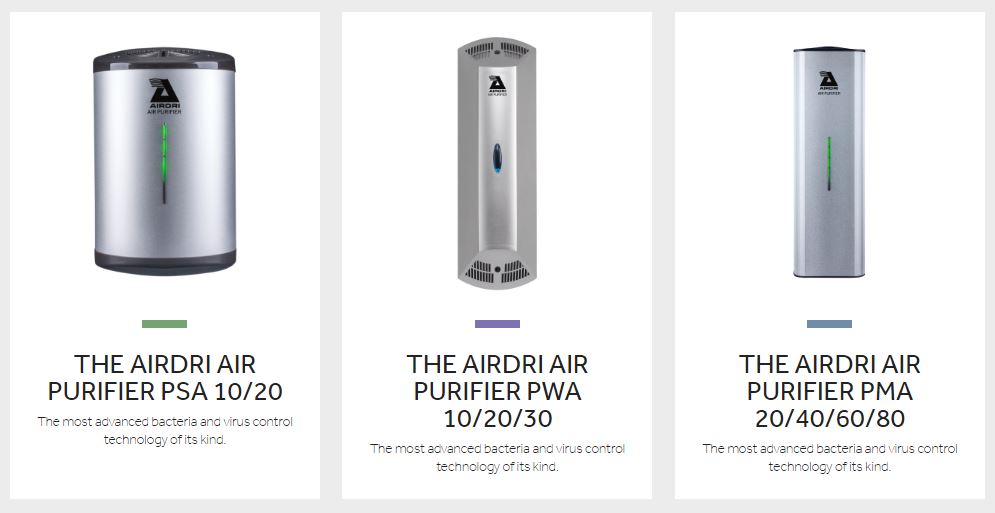
Odours are created by bacteria, viruses, mould, fungi and volatile organic compounds in the air and on surfaces. It is these odours that generate the perception of poor washroom hygiene. Tests carried out at Porton Down have proved that the Airdri Air Purifier kills 98.11% of all airborne and surface bacteria and viruses.
By killing harmful airborne and surface viruses and bacteria, the Airdri Thermal U/V Washroom Air Purifier eliminates odours from the washroom reassuring users that the washroom is clean. Regular cleaning and the use of disinfectants and masking agents cannot control the spread of micro-organisms however the Air Purifier can provide 24/7 infection and odour control by sanitising the air and all exposed surfaces.
- Completely silent
- Eliminates odours and mould
- Improves air quality
- Suitable for areas of continuous occupation
- Ideal for care homes, dental surgeries, waiting rooms, hairdressing salons, café and other hospitality uses
Contact: Airdri Ltd,
Technology House, Oakfield Estate,
Eynsham, Oxford, Oxfordshire, OX29 4AQ, UK
Telephone: +44 (0)1865 882330
Fax: +44 (0)1865 881647
Email: sales@airdri.com Website: www.airdri.com
Disinfecting premises using fog, mist, vapour or ultraviolet (UV) systems during the coronavirus outbreak

During the coronavirus (COVID-19) outbreak, fog, mist, vapour or UV treatments may be suitable options to help control the spread of the virus, by cleaning and disinfecting a larger space or room.
Any use of these treatments for these purposes should form part of your COVID-19 risk assessment. Users must be competent and properly trained.
Select the correct treatment
If you choose to use fog, mist, vapour or UV treatments as a way of cleaning and disinfecting surfaces, discuss your requirements with your manufacturers/suppliers (this may include fumigators), to help you decide if a product/system meets your needs. The treatment you use will depend on:
- the size of the area to be treated, its shape and how easily it can be sealed off if delivering an airborne product
- whether there are hard or soft surfaces – soft furnishings may act as a ‘sink’ for the airborne chemicals and emit them for some time after treatment (it may be possible to remove items such as sofas before treatment)
- the type of
business you have – some areas may be better suited to UV surface
treatments than airborne chemicals or vice-versa
Fog, mist, vapour method
If using the fog, mist, vapour method you will need to ensure the correct concentration of the active chemical is used, this means there is enough for it to work properly, but not so much as to leave a residue which may remain at unsafe levels for some time after treatment ends. There are different types of source disinfectants that can be applied as a fog, mist or vapour treatment. Some are liquid disinfectants used to create a fog, mist or vapour, such as hydrogen peroxide, others are generated from gases, for example ozone from air. Seek advice on what is appropriate to the environment that requires treatment.
UV method
An advantage of UV over disinfectants applied as a fog, mist or vapour is that no chemical residue is left behind. Rooms with complex configurations/interior designs may not be suitable for UV treatments due to the limitations of shadowing effects, unless multiple systems can be deployed. Similarly, very small spaces, such as small sanitary areas, may not be suitable for treatment via UV carousel as they need to be a minimum distance from walls etc to be deployed safely. Some disinfectant technologies are scalable so are typically more flexible in this respect.
Avoiding harm
Disinfectants applied as a fog, mist or vapour may reach harmful levels during delivery and UV systems may cause eye/skin damage if people enter an area undergoing treatment. Discuss with suppliers what safety features they can provide to prevent inadvertent access to a room during treatment. For example, safety sensors, simply locking rooms during treatment if feasible, or safety signage as part of a safe system of work.
Do not spray people with disinfectants
Spraying of individuals with disinfectants (such as in a tunnel, cabinet, or chamber) is not recommended under any circumstances. This practice could be physically and psychologically harmful and would not reduce an infected person’s ability to spread the virus through droplets or contact. Even if someone who is infected with COVID-19 goes through a disinfection tunnel or chamber, as soon as they start speaking, coughing or sneezing they can still spread the virus.
Do not disinfect large outdoor spaces
In outdoor spaces, large-scale spraying or disinfecting in areas such as streets or open marketplaces for the COVID-19 virus or other pathogens is not recommended. Streets and pavements are not considered as routes of infection for COVID-19. Spraying disinfectants, even outdoors, can be dangerous to people’s health and cause eye, respiratory or skin irritation or damage.
Supply and manufacture of disinfectants
The disinfectant applied as a fog, mist or vapour treatment must comply with the Biocidal Products Regulations (BPR). This includes the generation of ozone or free radicals. Please note the use of UV to disinfect is not covered by the BPR. Under BPR it is the disinfectant, or the chemical used to generate the disinfectant, added to the machine, that is the biocidal product. Please note that the machine itself is not covered by BPR. Suppliers of fog, mist or vapour units/machines should ensure that any disinfectant products they supply or recommend using with the unit/machine comply with BPR.
HSE has published separate guidance on the regulatory requirements for surface disinfectant products used, manufactured and supplied during the outbreak, which applies to disinfectant products applied via fog/mist/vapour units/machines.
Manufacturers of disinfectant products are responsible for ensuring that their products are suitably effective, including meeting any necessary testing standards. They are also responsible for providing information and instructions for the user on the product label.
The law on chemicals
Ensure that you follow the manufacturer’s instructions to ensure you are using the product safely and effectively. Where units/machines are used in a workplace, under the Control of Substances Hazardous to Health Regulations (COSHH) employers must ensure substances which may be harmful to people’s health from their work activities are identified and assessed; and processes are put in place to eliminate or control risks.
COSHH also requires employers to provide information, instruction and training for all their employees who use hazardous substances such as disinfectants in their work, including the appropriate precautions and actions employees must take to safeguard both themselves and others in the workplace.
Sealing off rooms
Rooms treated by UV or disinfectants applied as fog, mist or vapour should be empty and sealed off to avoid risk of human exposure to the potentially harmful treatments. Disinfectants may reach harmful levels during delivery and UV systems may cause eye/skin damage if people enter an area undergoing treatment. You may also consider safety sensors that can shut off UV systems if a room is inadvertently entered during treatment.
Rooms that are very difficult to seal may not be suitable for delivering airborne chemicals.
Social distancing and making your workplace COVID-secure

Social distancing means keeping people apart to help reduce the spread of coronavirus.
Where possible you should keep people 2m apart. If this is not viable, keeping 1m apart with risk mitigation is acceptable.
In the UK some rules such as social distancing may be different in each of the devolved nations. However, HSE regulates in all of these countries. You should check the public health guidance for the country you are in:
You must ensure that workers and other people visiting your workplace understand and comply with the measures you put in place.
Social distancing should form part of your business’s risk assessment and is one of the steps needed to make your workplace COVID-secure.
The gov.uk guides on working safely during coronavirus (COVID-19) explain the control measures that different types of business should consider. These cover construction, factories, offices, vehicle use and other types of work. The guides apply to workplaces in England.
The following guidance sets out the main control measures and additional measures where social distancing is not possible:
- Common areas (includes break areas, bathrooms, toilets, meeting rooms and accommodation)
- Workstations
- Arriving and leaving work
- Movement around buildings and worksites
- Where 2m social distancing is not possible
- Using vehicles
- Emergencies, security and other incidents
Common areas (includes break areas, bathrooms, toilets, meeting rooms and accommodation)
Common areas are used by many people. The potential for spread of coronavirus is considered to be higher in these areas if proper controls are not in place.
Identify and review the common areas within your workplace including:
- restrooms
- kitchens
- tea points
- changing facilities
- lifts
- meeting rooms
- smoking areas
- canteens
- toilets
- showers
- reception areas
- accommodation
Also consider pinch points in your premises such as narrow corridors, staircases, doorways and storage areas.
You may need to put in place a combination of control measures to keep people safe.
General control measures
Consider putting the following control measures in place for common areas:
- Limit the number of people at any one time using any areas that may become congested.
- Use floor markings to maintain social distancing.
- Keep surfaces clear so that cleaning can be carried out more effectively.
- Identify objects that may be touched more frequently, such as kettles, cooking equipment, phones, computers or tables and make sure that they are frequently cleaned.
- Try to maximise ventilation.
- Make sure that your workforce is clear on the rules when using common areas.
- The areas should be regularly cleaned in line with your cleaning plan.
- Minimise contact between people, using barriers or screens.
- Provide hand-washing facilities or hand sanitiser near to frequently used areas.
- Display signs reminding people to socially distance, wash hands and not touch their faces.
- Work with landlords and other tenants in multi-tenant sites or buildings to ensure consistency across areas such as receptions and staircases.
Guidance on cleaning, hygiene and hand sanitiser.
Break areas
Employers must make sure all workers, including those visiting your premises for work, have somewhere to rest and eat and should also provide facilities to heat food or water for hot drinks. Find out more about having the right workplace facilities.
Consider these control measures:
- Ensure that workers understand the need to maintain social distancing and good hand hygiene before entering any areas where food is consumed.
- If workers need to leave the site at break times remind them to maintain social distancing while off-site.
- If canteens are used, consider if food, cutlery etc can be delivered to tables. Where canteens need to serve food reconfigure seating and tables to maintain spacing and reduce face-to-face interactions. Mark the floor in case furniture is accidentally moved.
- Stagger or extend break times to limit the numbers of people using the facilities.
- Create additional break areas where required such as in unused rooms. It may be possible to create outside break areas where it is safe to do so.
Bathrooms, toilets and washbasins (welfare facilities)
You have a legal duty to provide adequate toilet and washing facilities that are easy and safe to access. This applies to any workers (including those not employed or contracted to you), and visiting workers who are not normally on your premises. The legal responsibility to provide access to these facilities lies with whoever controls the premises.
Refusing access for any reason, including as an infection control measure, is against the law. It is vital that people can wash their hands regularly, so not allowing access to welfare facilities may increase the risk of COVID-19 spreading.
When completing your COVID-19 risk assessment, review the provisions you have to make sure they allow people (including visiting workers) to social distance, use the toilets and wash hands frequently. Consider whether you need to provide any additional washing facilities.
To protect people when using existing toilet and washing facilities consider the following:
- Identify all surfaces that require additional cleaning in bathrooms and toilets.
- Taking some static facilities out of use where they are less than 2m apart. If this includes toilet facilities such as urinals you should ensure that you still have a sufficient number of toilets in your workplace.
- Put markings on floors to show people the right distances or where to stand.
- Put in place systems such as ‘one in, one out’ if it isn’t possible to maintain social distancing.
- Make sure you provide running water and soap to enable people to clean their hands properly.
- Provide hand drying facilities – paper towels or hand dryers.
- Empty bins frequently to safely dispose of waste. Where possible have open-topped bins or foot operated lids.
- Using signs and posters to increase awareness of good handwashing technique.
- Decide how and when handwashing facilities will be cleaned and when bins will be emptied.
- Decide who will replenish soap, paper towels and hand sanitiser.
Guidance on cleaning, hygiene and hand sanitiser.
Additional handwashing facilities
When completing your COVID-19 risk assessment, consider if you need to provide additional handwashing facilities so that people can wash their hands frequently.
Consider:
- where people work
- how much contact they have with others
- the frequency they should wash their hands as a result
This will also help you to decide if and where you need to provide additional washing facilities.
If you cannot provide additional handwashing facilities, you may need to provide hand sanitiser instead in some circumstances.
When you complete your risk assessment, think about:
- providing handwashing facilities at entry and exit points so people can wash their hands when they arrive and leave work – if this is not possible, provide hand sanitiser
- where extra handwashing facilities need to be to allow people to wash their hands frequently
- making sure your handwashing facilities have running water, soap and paper towels or hand dryers
- identifying where extra hand sanitiser points are needed in addition to washing facilities
Meeting rooms
Consider the following measures:
- Use remote working tools to avoid in-person meetings.
- That only absolutely necessary participants should physically attend meetings and should social distance throughout.
- Avoid sharing pens, documents and other objects.
- Provide hand sanitiser in meeting rooms.
- Hold meetings outdoors or in well-ventilated rooms whenever possible.
- For areas where regular meetings take place, using floor markings to help people maintain social distancing.
Accommodation
Employers who provide accommodation for their workers should consider the following:
- Identify measures to keep workers safe while they are staying in accommodation and working, in your risk assessment.
- Minimise numbers of people living in shared accommodation.
- Treat each accommodation living unit (eg caravan) as a ‘household’.
- How you will ensure if one person in the ‘household’ shows symptoms that all will self-isolate in line with the guidance for households with possible coronavirus infection.
- Workers should not live or stay in more than one ‘household’.
- Keep people who live in the same household together in the same work group.
- Try not to mix households while they are working.
- Try to keep each household socially distanced from other households.
- Check workers health before they start work each day.
- If a worker develops symptoms of coronavirus while working they should return to their household. The individual, and anyone else highlighted by government guidance should then follow the government guidelines on isolation.
- Cleaning regimes to ensure accommodation units stay clean.
- Cleaning regimes for shared communal areas. The employer is responsible for making sure that communal areas are properly and regularly cleaned.
- Carryout statutory checks such as landlord gas safety checks as required.
- Cleaning and maintenance regimes for toilets and showers.
- Provide fire safety precautions as normal.
Workstations
Workstations are areas where workers routinely or regularly work and can include:
- desks or tables in the workplace
- production or processing lines
- areas by machinery that workers need to operate
- desks within workers homes if they are working at home
- vehicles
Consider the following:
- Look at how you can organise workstations to allow people to meet social distancing rules.
- Review layouts and processes to allow people to work 2m apart from each other where possible.
- Use floor tape or paint to mark areas.
- Manage occupancy levels.
- Avoid any sharing of workstations, including hot desking where possible.
- Limit the number of people having to share a workstation to the absolute minimum.
- Where workstations must be shared, try to keep the same set of people using them.
- Make sure that workstations are cleared at the end of the day or shift so that they can be properly cleaned.
- Ensure that all workstations are regularly cleaned in accordance with your cleaning plan.
Where it’s not possible to keep workstations 2m apart, consider these additional control measures.
Guidance on cleaning, hygiene and hand sanitiser.
Arriving and leaving work
Consider these control measures for when people are arriving or leaving work:
- Take precautions to limit the chances of anyone with coronavirus entering your premises, for example, display signs asking people not to enter your workplace if they have symptoms of coronavirus.
- Limit the number of people entering your workplace, or parts of your workplace, to avoid overcrowding. Think about if you can you arrange partial working from home for some staff.
- Stagger arrival and departure times to reduce crowding into and out of the workplace, taking account of the impact on those with protected characteristics.
- Provide additional parking or facilities such as bike racks to help people walk, run, or cycle to work where possible.
- Provide more entry points to reduce congestion.
- Provide more storage for workers for clothes and bags. Encourage storage of personal items and clothing in personal storage spaces, for example lockers during shifts.
- Use markings and introduce one-way flow at entry and exit points.
- Provide handwashing facilities at entry and exit points, or hand sanitiser where handwashing is not possible. Make sure you provide these facilities for anyone entering your workplace.
- Where possible, avoid using touch-based security devices such as keypads. If you need to use them, make sure they’re cleaned regularly.
- Where possible, introduce shift working to limit the number of people in the workplace at any one time. This may also reduce the burden on public transport if your employees use it to travel to work.
- Where possible, introduce suitable barriers or screens where people regularly interact, such as service desks or reception areas. If used, ensure they are cleaned and disinfected in line with your cleaning procedures.
- Put in place procedures for dealing with deliveries and visitors. Allocate time slots for customers.
- Put in place measures to keep delivery drivers safe, this includes allowing delivery drivers to use welfare facilities.
Guidance on cleaning, hygiene and hand sanitiser.
Movement around buildings and worksites
Consider these control measures when people are moving around buildings or worksites:
- Use floor markings to mark out social distancing. Focus particularly on the most crowded areas, for example where queues form, entry points to buildings, toilets and communal break areas. Additional control measures may be needed for areas at higher risk of overcrowding, such as common areas.
- Use any unused spaces to allow people to spread out and comply with social distancing rules.
- Reduce movement by discouraging non-essential trips within buildings and sites, for example restricting access to some areas, encouraging use of radios or telephones or other electronic devices, where permitted, and cleaning them between use.
- Restrict access between different areas of a building or site.
- Reduce job and location rotation.
- Introduce more one-way flow through buildings.
- Reduce maximum occupancy for lifts. Provide hand sanitiser for the operation of lifts. Encouraging use of stairs wherever possible.
- Make sure that people with disabilities are able to access lifts.
- Manage the use of high-traffic common areas including corridors, lifts turnstiles and walkways.
- Put in place measures to remind staff and visitors to follow social distancing.
Where 2m social distancing is not possible
Consider these additional control measures where 2m social distancing is not possible:
- Consider if the activity needs to continue or if it can stop.
- Keep the number of people working who cannot social distance to a minimum.
- Reduce the number of people in close proximity in the work area.
- Limit the movement of people around the site. Consider if workers stay in one place, or at one workstation when working.
- Limit the amount of different equipment or surfaces that people need to touch.
- Assign workers to teams which then socially distance from other teams. Keep workers in the same teams as far as possible to limit social interaction. Keep teams as small as possible. If a team member becomes ill with symptoms of coronavirus, they and the rest of the team should follow the UK government guidance on self-isolation.
- Use screens between people to create a physical barrier. You should keep the screens clean.
- Organise the space so that people are side-by-side or facing away from each other rather than face-to-face.
- Mark the floor of areas such as lifts to show where people should stand and what direction they should face.
Guidance on cleaning, hygiene and hand sanitiser.
Using vehicles
On gov.uk there is guidance for people who work in or from vehicles setting out control measures to help protect workers.
Consider the following control measures:
- If travel in vehicles is needed for the business to continue to operate.
- Ensure those who are travelling are necessary for the work to be carried out.
- Limit passengers in corporate vehicles such as work minibuses. This could include leaving seats empty.
- Consider if social distancing measures can be implemented in the vehicle.
- Avoid multi-occupancy vehicles where safe to do so.
- Where multi-occupancy vehicles are used, people should social distance where possible through suitable seating arrangements and where necessary, use of additional transport. Keep the journey as short as possible.
- Where more than one person is travelling and they need an overnight stop, plan ahead to ensure there is suitable accommodation secured to ensure social distancing.
- Consider if people who need to travel in vehicles can be kept in the same teams.
- Consider if vehicle windows can be kept open.
- Ensure that people practice good hygiene before and after using the vehicle. Provide hand sanitiser where necessary.
- Vehicles should not be shared between different users if possible.
- Remind workers to travel alone to and from work where possible, either in their own transport, by walking, or cycle if it is safe to do so.
- Ensure vehicles are cleaned regularly, in particular between different users. Clean commonly touched areas in vehicles including:
- handles (inside and out)
- steering wheel and starter button
- centre touchscreen and stereo
- handbrake and gearstick
- keys and key fob
- indicators and wiper stalks
- windows, mirrors and mirror switches, seat adjusters any other controls
Where it’s not possible for people to social distance in a vehicle, consider additional measures such as:
- using physical screening, as long as this does not compromise safety, for example by reducing visibility
- sitting side-by-side not face-to-face
- using a fixed pairing system if people have to work in close proximity
Drivers’ welfare at delivery and collection sites during the coronavirus (COVID-19) outbreak
Emergencies, security and other incidents
Consider the following:
- Reviewing your incident, first aid and emergency procedures to ensure people can social distance as far as possible.
- Considering the security implications of any changes you intend to make to your operations and practices in response to the coronavirus outbreak as any revisions may present new or altered security risks.
- For organisations who conduct physical searches of people, considering how to ensure safety of those conducting searches while maintaining security standards.
Public Lavatories Bill unanimously passes second reading in Parliament

Minister Simon Clarke MP, from the Ministry of Housing, Communities and Local Government presents the Non-Domestic Rating (Public Lavatories) Bill 2019-2021 to the House of Commons today. The Bill received unanimous approval, for adoption, by the ministers present. When brought into legislation it will effectively remove the levy of (NDR) Rates from all “stand-alone” public toilets in England and Wales. The devolved administrations will be expected to adopt the new Act.
The Hansard Transcript of the proceedings can be read in full by following this LINK:
The BTA is delighted to annoounce the long awaited progress of the NDR Bill to remove the rates levy from all “stand-alone” public toilets. Our founder and current President Richard Chisnell took up this baton in 2012 and it has been an arduous journey through the years to get to this point. In 2015 the BTA board agreed to make this relief a priority and Roger Berry took the lead in speaking to likeminded organisations and political colleagues to try and move the proposal forward.
October 2018 the Chancellor of the Exchequer Mr Philip Hammond announced, during his budget speech, in Parliament that he was introducing the NDR Public Lavatories Bill and following the Bill passsing through the House of Lords and the House of Commons we’re almost there.
The Bill will now go forward immediately after the summer recess of Parliament and be laid before the House of Lords for their final approval before hopefully progressing to Royal Assent to become an Act of Parliament and enter into our Primary Legislation.
Local Authorities will be able to claim a FULL rates allowance relief on all Publicly Accessible Toilets under either their or even private control and use the monies saved to upgrade their services and provision of existing facilities. The minister thanked a number of organisations including the BTA, NALC and RSPH for their support and help in campaigning for this change in future legislation.

Thangam Debbonaire, the Shadow Secretary of State for Housing, lead those ministers present in congratulating Mr Clarke for presenting the Bill and the government for strongly supporting its immediate adoption – but suggested that there were still further enhancements called for. She agreed that this was a great first small but important step to retaining and restoring these essential buildings – but asked if government could look at the numbers of toilets lost over previous years and perhaps use some Covid emergency funding to redress the loss. Many public buildings, such as libraries, museums ansd civic centres were excluded under this pending legislation and she again asked if consideration might be given to how these additional local amenieties could be included, at some future juncture.
The Minister also proposed that, due to the keen support from many ministers and colleagues, that a working group should be established to look at the wider range of issue around provision of Public Toilets for all citizens, especially those with severe medical, emotional and physical conditions who relied daily on finding urgent relief when moving away from home. Ministers highlighted the plight of all those persons working away from their bases, lorry, coach, bus and taxi drivers and alos those in emergency services and social care who rely on these essential facilities. The Minister kindly thanked the BTA for providing some information and guidance on the essential and vital role played by publicly accessible toilets throughout society and the nation.
With the increased demands being placed upon these vital provisions following the easement of lockdown it is now critical that we see immediate investment in upgrading and reopening these frontline services. As we try to rebuild our local economies and invite tourism back to our towns and villages were have to invest time, money and expertise in getting our publicly accessible toilets hygienically cleaned and safe for use.
Both Minsters praised the national Changing Places programme and the work that BTA have been committed to with Muscular Dystrophy UK and Pamis in Scotland; in creating the CP Map and identifying potential new sites. Substantial funding of £30million has already been agreed to expand the reach of this programme and to greatly increase the number of sites where these specialised rooms can be best utilised.
The British Toilet Association wishes to thank all those individuals, groups and organisations who have worked closely with ourselves and our member organisations over the years to help bring about this relief legislation to local authorities.
We offer our special thanks to everyone who continues to fight tirelessly for the national retention of publicly accessible toilets and the future upgrading of our “away-from-home” toilets and the increasing standards of hygiene and provision — for ALL USERS.

CHANGING PLACES CAMPAIGN
The BTA Director and the Board are fully committed to working with our colleagues in the Ministry of Housing, Communities & Local Government, Muscular Dystrophy and Pamis to support, maintain and expand the Changing Places Campaign, the CP Mapping System and the continued natonal drive for NEW facilities.